Book Your Free Consultation
Mr David Allamby
MD, FRCOphth, FRCS
The Complete Patient's Guide To Cataract Surgery
This is a complete guide to cataract surgery.
In this in-depth guide, you will learn;
We’ll also look at the procedure and the implant choices available.
So, if you’re ready to learn everything about cataract surgery, let’s jump straight in!

CHAPTER 1
Cataract refer to cloudy changes in the lens of the eye. This lens sits just behind your pupil, the black opening in the centre of your coloured iris.
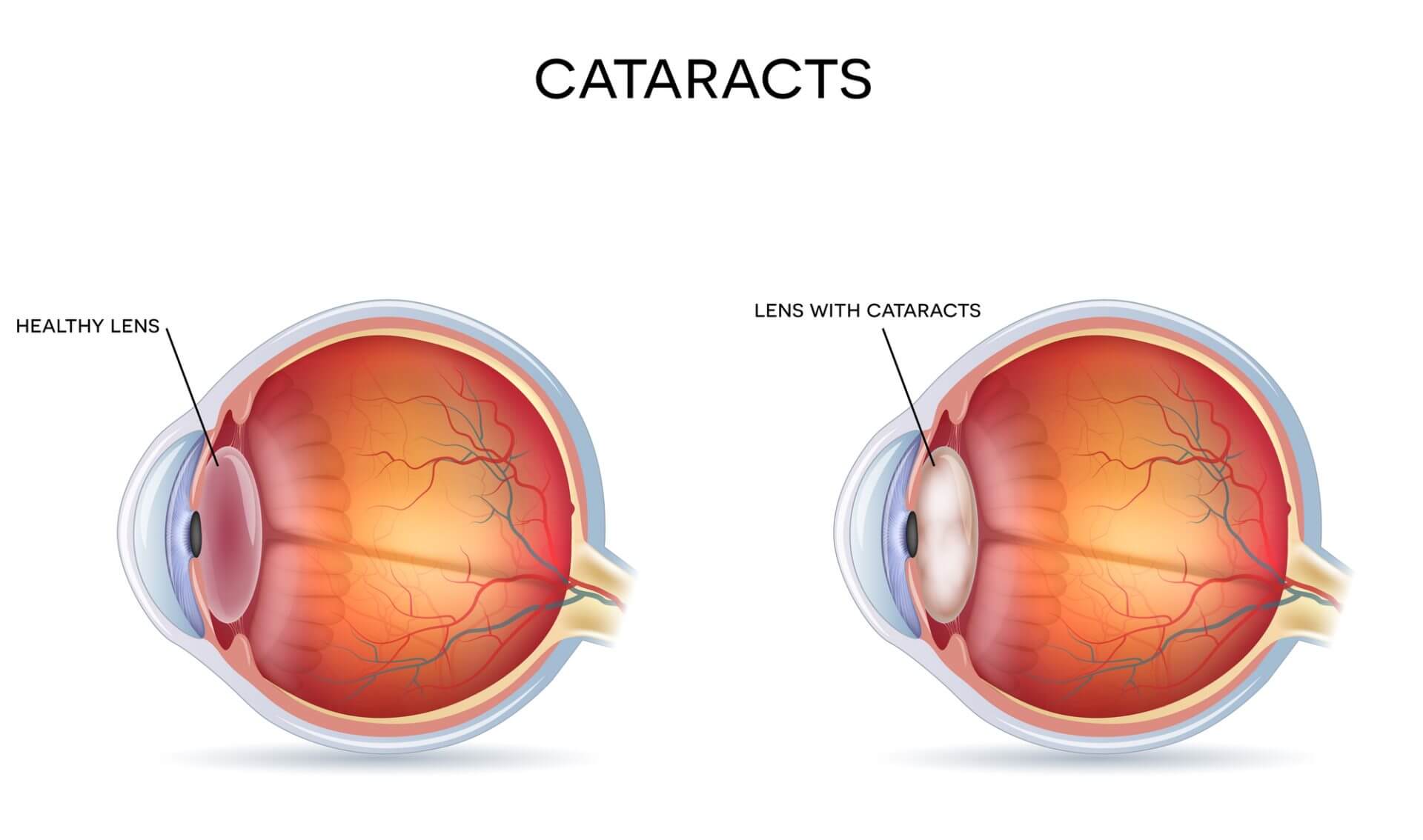
In the healthy eye, light enters through the cornea (the transparent window at the front of the eye), then passes through the pupil and the lens. The lens helps focus light rays on to the light-sensitive cells within the retina at the back of your eye.
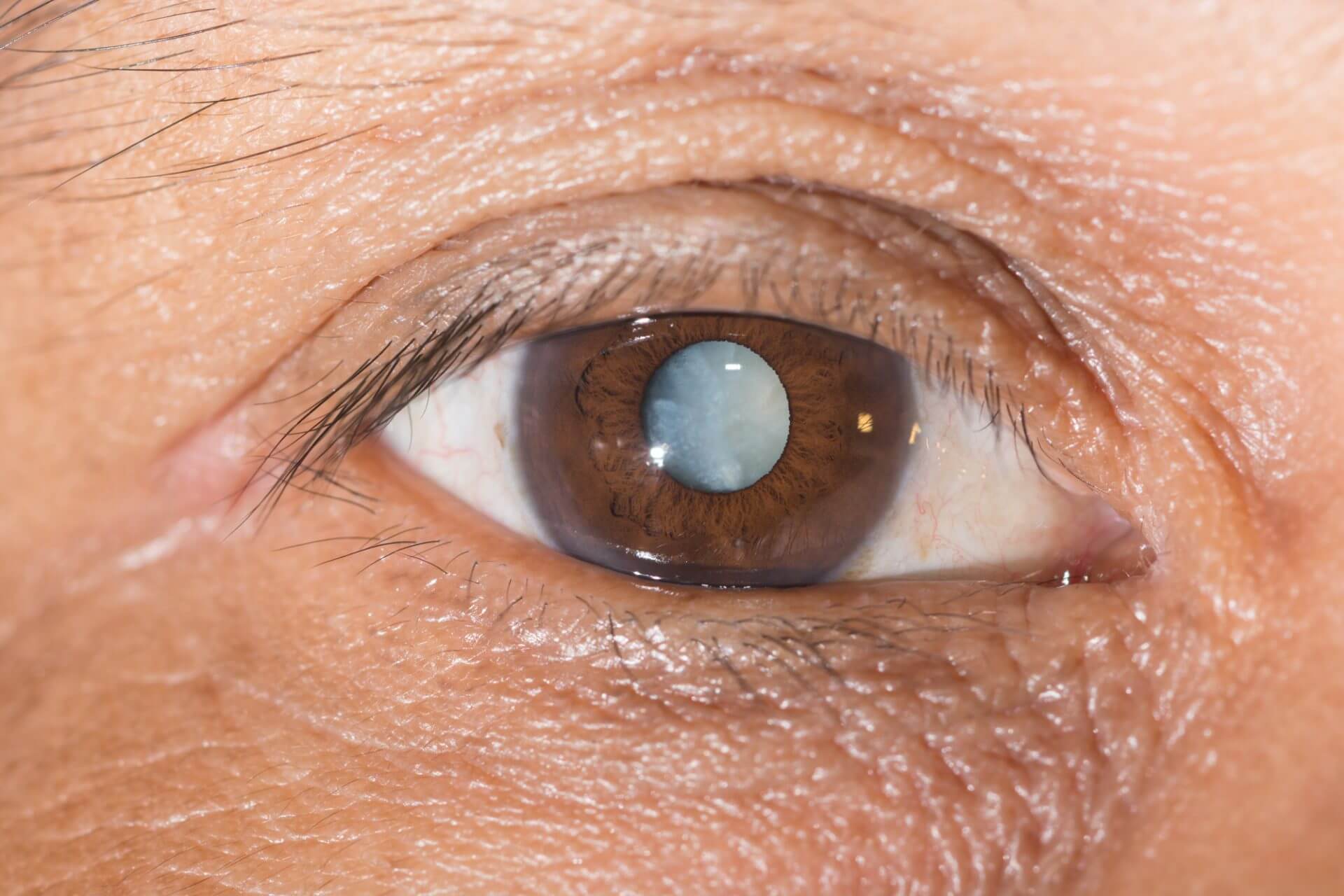
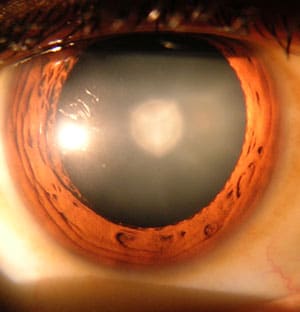
When a cataract forms, the normally clear lens develops semi-opaque or fully opaque areas causing it to become less transparent. Lens opacities range from minimal to advanced and, in the worst cases, create an entirely white lens. Over months or years, cataracts become worse and start to affect vision. Eventually, surgery will be required to remove and replace the lens. Glasses will not correct the problem.
Cataracts are most commonly as a result of ageing and become increasingly prevalent after the age of 60.
The word cataract comes from the Latin cataracta meaning ‘waterfall or floodgate’ and refers to the white appearance of the pupil in advanced cataracts.
It is rare to see such advanced ‘mature’ cataracts in the developed world, but they are not uncommon in developing countries.
CHAPTER 2
The North London Eye Study found that the prevalence of cataract increases with age.
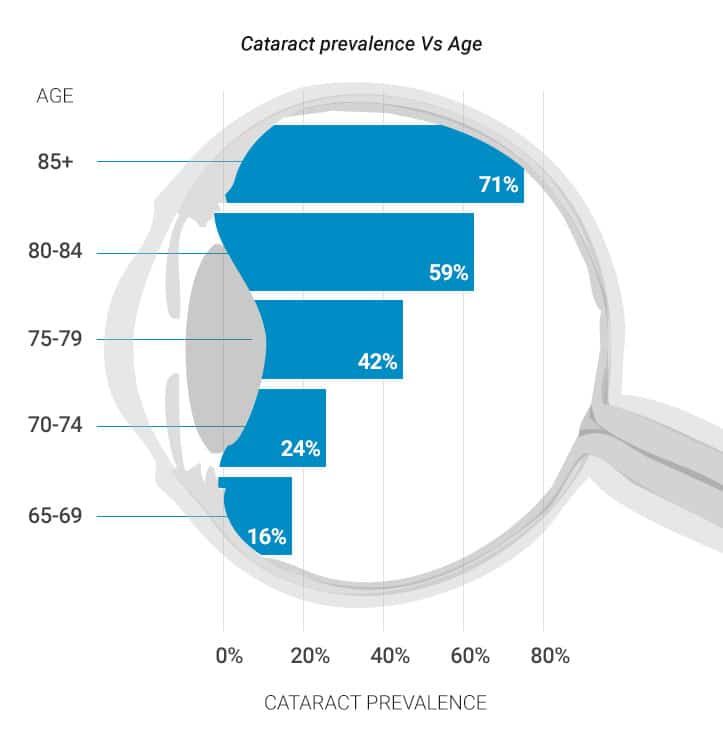
In the UK, age-related cataracts will affect around 20% of those aged 70. This rises quickly to 50% by 80 years old and just over 70% of those aged 85 or older.
“Half of all people will have cataracts by age 80, rising to 70% by 85” North London Eye Study
CHAPTER 3
The most common cause for cataracts is ageing.

CHAPTER 4
There are multiple types of cataracts, depending on the location of the opacity within the lens. Some are very slow to develop, gradually reducing vision over a number of years, whereas others can progress more quickly, even within weeks or months.
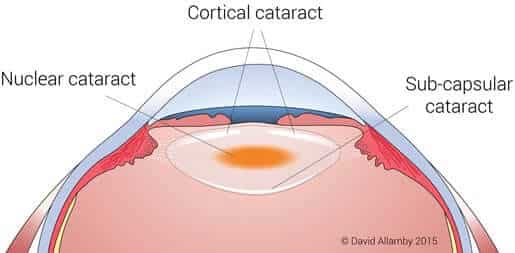
The most common types of cataract are:
Subcapsular cataract
Appear at the back of the lens and often produce initial problematic symptoms of glare from bright lights, e.g. car headlights, before progressing on to general vision reduction. People with diabetes or those taking high doses of steroid medications have a greater risk of developing a subcapsular cataract.
Nuclear cataract
Are most commonly associated with ageing. These central lens changes start as a yellowing deep in the central nucleus of the lens, later becoming brown (known as lens brunescence). They cause a general reduction in visual clarity and a yellow hue to colours.
White, spoke-like opacities found in the lens cortex, the outer part that surrounds the nucleus. Cortical cataracts begin in the periphery and then progress inwards to the centre.
CHAPTER 5
Cataracts can develop over months or more commonly years and, initially, they may present no symptoms. They usually affect only a small part of the lens in the early stages but will progress and extend over time.

Lens Replacement Surgery Cost
Cataracts may develop in one eye at first, but very typically go on to affect both eyes.
Cataracts are not painful or itchy. The eyes are not red or inflamed, and will usually appear normal. In very advanced cataracts, the pupil may become grey or white (the white appearance was likened to a waterfall, from where cataracts get their name).
The location of the cataract will determine the kinds of symptoms you will experience:
Nuclear cataract often leads to an improvement in near vision because of an increase in short-sightedness. The patient may feel their eyesight is actually getting better though, as the cataract progresses, vision will become worse.
Cortical cataract may not produce any symptoms until it extends centrally and reaches the visual axis within the pupil. At this point vision will quickly deteriorate.
Subcapsular cataract may produce little in the way of symptoms until it becomes quite advanced, although there may be early effects of glare from bright lights.
Symptoms of Cataracts
CHAPTER 6
A cataract is an abnormal opacity in the naturally clear natural lens inside the front part of the eye. The most common reason is ageing, though there are many other factors which have been linked to their development.
The role of the lens is to help light focus onto the retina at the back of the eye. When we are young, it is a flexible gel, able to change its shape through the action or a ring of muscle within the eye (ciliary muscle). The lens can become either flatter or rounder, allowing us to focus at almost any distance, from far to near.
The components of the lens are mainly proteins and water, arranged as regular clear fibres in concentric layers, rather like an onion. The arrangement of these fibres and proteins is very precise, resulting in transparency that lets light pass through the lens and also focused to form an image on the retina.
The primary cause of cataracts, while not fully understood, appears to be clumping together of proteins, with unequal distribution of protein and water within the lens. This clumping can lead to a small area of opacification which can extend over time as the patient ages. As this clouding increases and affects the line of sight in the central lens, vision is affected.
Causes of Cataracts;
CHAPTER 7
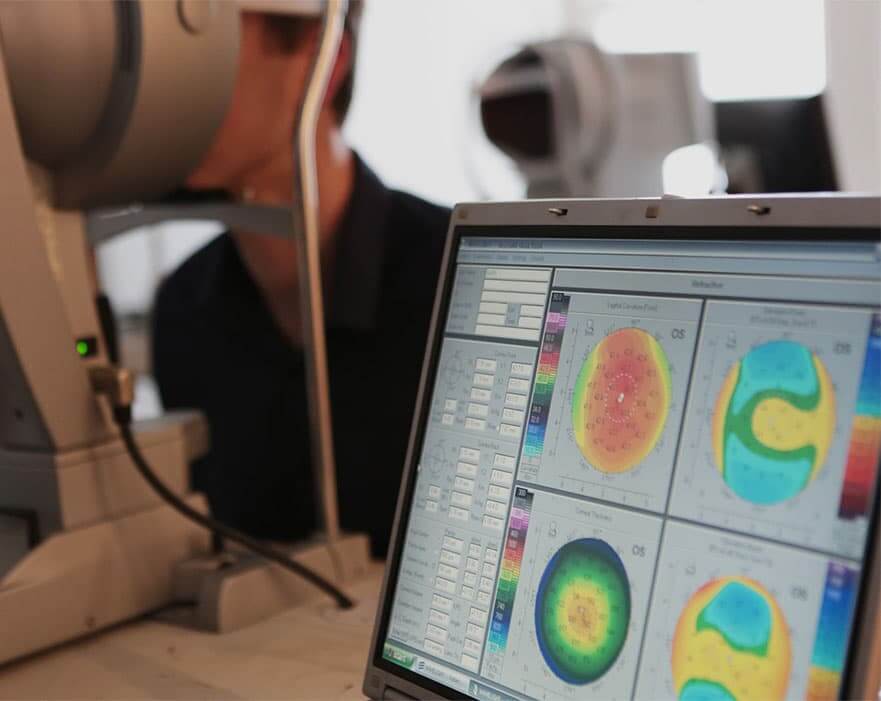
If you have noticed problems with your sight, the first step is to see your optician or optometrist. They can examine your eyes, confirm your prescription and test your vision.

The optometrist will use a microscope known as a slit lamp or a hand-held ophthalmoscope. These specialist instruments give a magnified view to look inside your eyes and check for cataracts.
If lens opacities are found you will be referred to an eye surgeon (ophthalmologist), who specialises in cataract surgery. They can confirm the diagnosis and describe how cataracts are typically removed under a local anaesthetic in a 10-15 minute procedure.
Cataract surgery in the UK is either performed by the NHS or as a private patient. The advantages of a private procedure is the ability to upgrade to a premium multifocal lens implant (IOL) that can help restore reading vision as well as distance sight.
CHAPTER 8
There is controversy about whether cataracts can be prevented, as no studies to date have demonstrated how to avoid or slow their progression. There may be a number of approaches that might be of help in reducing your risk of cataracts:
Regular eye examinations can help detect cataracts and other issues before they become a problem.
If you are 45+ you should have an eye test every two years, or yearly if you are at increased risk, e.g. a close family member having glaucoma.
Reduce alcohol intake, as we know that excessive consumption can increase the risk of cataracts.
Wear sunglasses that block 100% of ultraviolet (UV) rays when you’re outdoors, as UV radiation from the sun may contribute to the development of cataracts.
Carefully control other health issues, especially if you have diabetes or other medical conditions that can increase your risk of cataracts. Keep to a healthy weight.
A healthy diet that includes fruits and vegetables could potentially reduce your risk of cataracts. Fruits and vegetables contain antioxidants, which may help maintain the health of your eyes.
Stop smoking, as it increases the likelihood of developing cataracts, as well as a wide range of other health issues
CHAPTER 9
A healthy diet that includes fruits and vegetables could potentially reduce your risk of cataracts. Fruits and vegetables contain antioxidants, which may help maintain the health of your eyes.

Although research studies have not shown that antioxidants supplements in pill form can help in preventing cataracts, a large study recently showed that a diet rich in vitamins and minerals was associated with a reduced risk of developing cataracts.
Increasing the amounts of fruit and vegetables in your diet can have several health benefits. Vitamin E, lutein and zeaxanthin may be beneficial to eye health.
Food sources rich in vitamin E include sunflower seeds, almonds and spinach. Lutein and zeaxanthin can be found in kale, spinach, and other leafy green vegetables.
CHAPTER 10
Cataract surgery is very effective in restoring vision. Most patients undergoing the procedure return to having very good sight.

When symptoms of cataract begin to appear, you may be able to help your vision for a period by using new (stronger or even weaker) glasses, magnifying glasses for certain tasks, better lighting or other aids to improve vision.
The time for surgery is when cataracts have advanced sufficiently to impair your eyesight and negatively affect your daily life.
Poor vision is not an inevitable part of getting older. Cataracts are the most common cause of reversible vision loss in the UK, and cataract surgery is a simple procedure to regain vision. Surgery is usually a walk-in, walk-out day case procedure using a local anaesthetic.
CHAPTER 11
Cataract extraction with intraocular lens implant for age-related cataract is the most frequent surgery performed in the NHS.
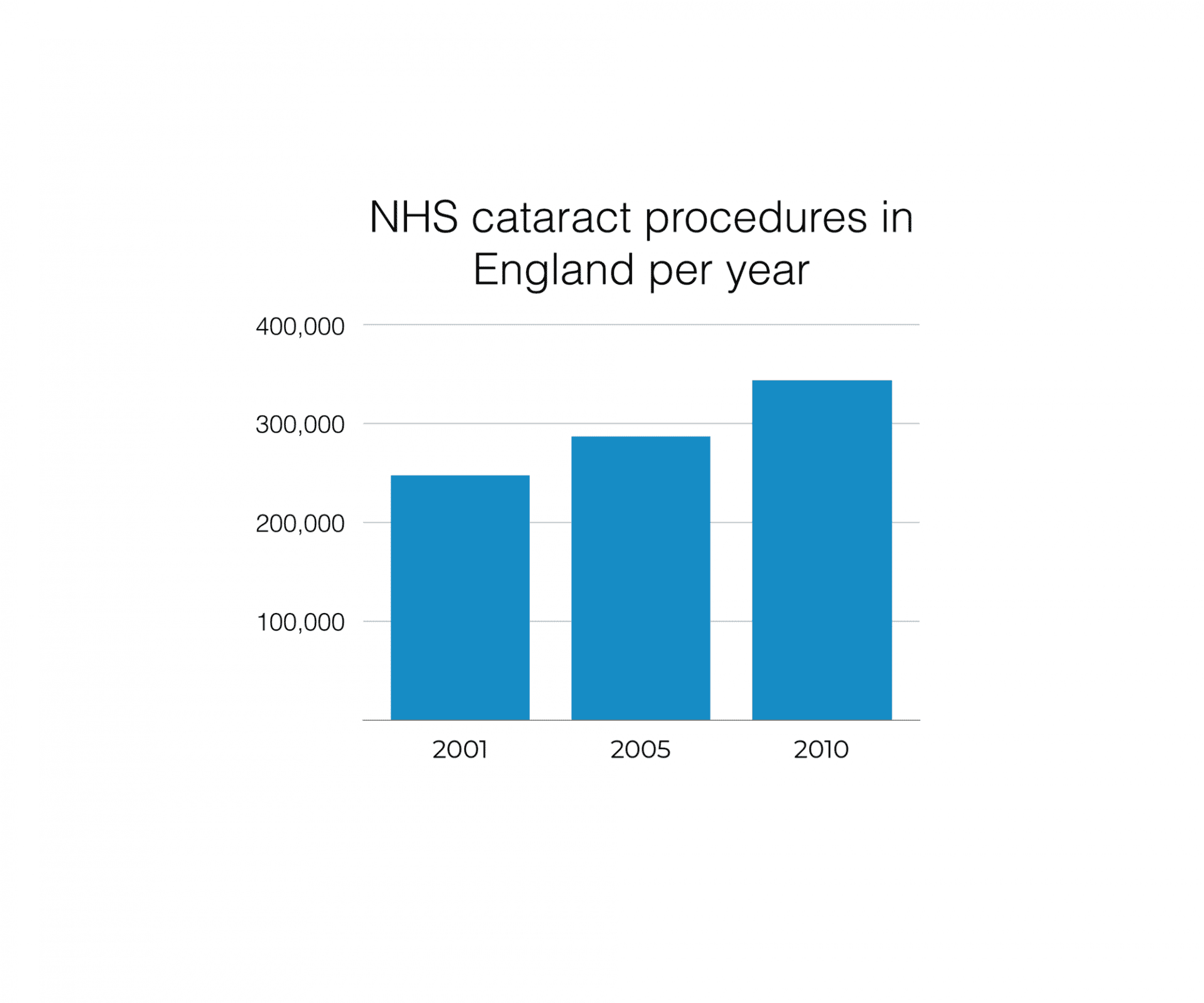
There were 337,000 cataract operations in England in 2011/12, with 98 percent carried out as day cases.
The average age for those undergoing a cataract operation on the first eye was 77 years, with 95% of cataract operations being carried out from a waiting list. The average waiting time was 65 days.
Over the last decade, there has been a significant increase in the number of cataract operations performed by the NHS in England. There are now almost 100,000 more cataract operations than a decade ago, an increase of 39% over this period.
CHAPTER 12
Source: The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery;
CHAPTER 13
Cataract surgery involves removing the cloudy lens through a small incision in your eye and replacing it with a clear, plastic one, known as an intraocular lens (IOL). In most cases, the procedure is carried out under local anaesthetic (where you’re conscious, but the eye is numbed) and you can usually go home the same day.

Almost everyone who has cataract surgery experiences an improvement in their vision, although it can take a few days or weeks for your sight to settle. You should be able to return to most of your normal activities within about two weeks.
After the operation, your plastic lens will be set up for a certain level of vision, so you may need to wear glasses to see objects that are either far away or close. If you wore glasses previously, your prescription will probably change. However, your optician will need to wait until your vision has settled before they can give you a new prescription.
If you have surgery privately, you will have the option to upgrade to premium multifocal implants. These advanced lenses are designed to give clear intermediate (computer range) and close (reading) vision, as well as good distance sight. See the section on A Revolution in Lens Choices for more information. In a private setting, the eyes will usually be treated one week apart, whereas in the NHS or other universal healthcare setting, the delay can be considerably longer.
CHAPTER 14
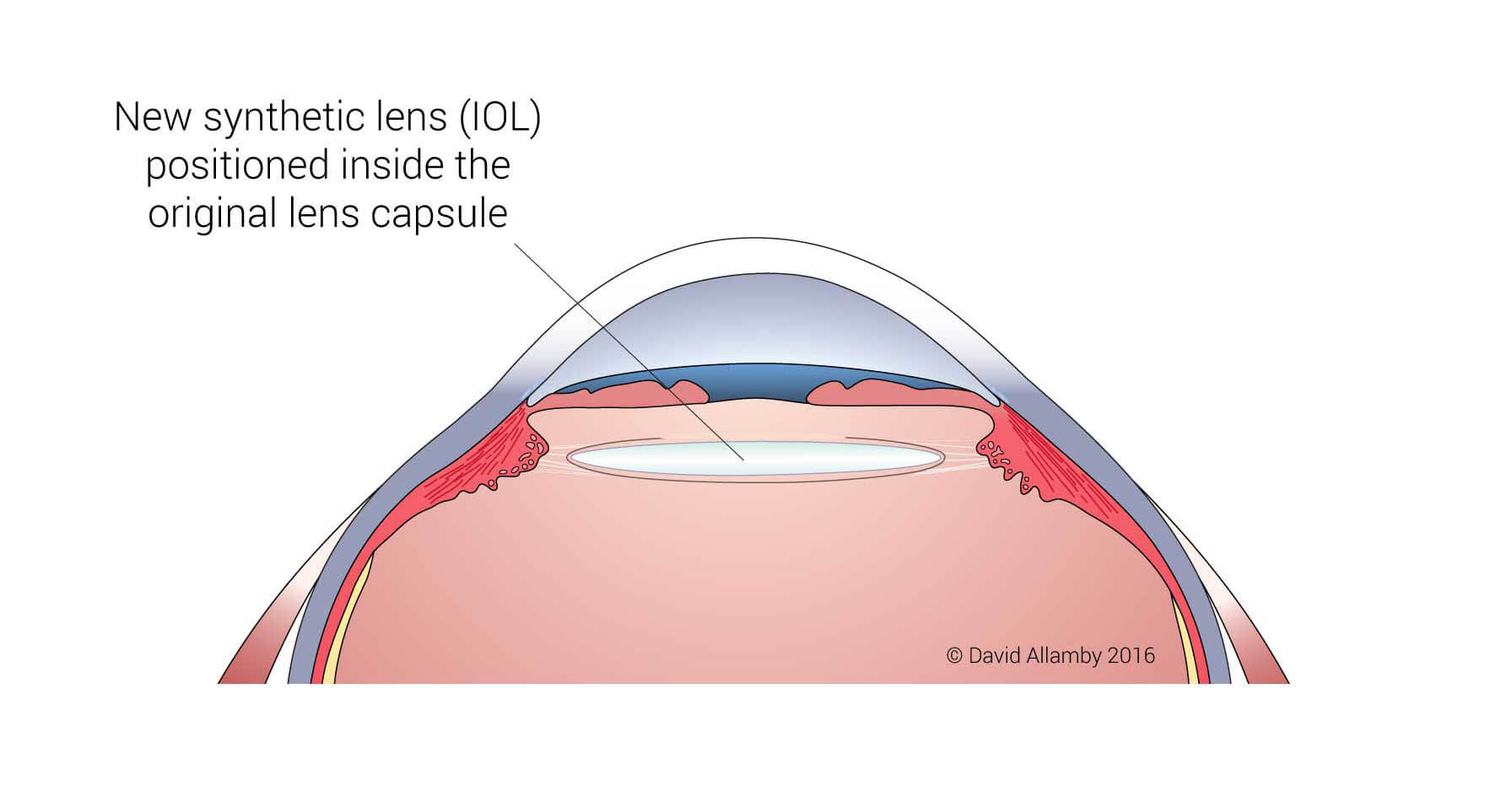
The surgical approach for the various types of cataract is the same and involves 3 main steps. It will remove both the central nucleus and lens cortex. Hence any lenticular opacity it will be removed during the extraction of the natural lens, irrespective of its location.
Removing the nucleus and surrounding cortex will leave the lens’ clear surrounding bag in place, known as the capsule. An intraocular lens (IOL) implant is placed within this remaining capsular bag.
The power of the lens is calculated to restore clear distance vision. Reading (30 to 50 cm away) and intermediate (~60 cm to 1.0 metre) vision can also be provided through the use of a premium multifocal or accommodating IOL. Trifocal IOL designs are increasingly popular.
CHAPTER 15
Cataract Surgery: Step 1
The first step after anaesthetising the eye is to remove the cloudy cataract lens from behind the iris. Tiny keyhole entrance points are made at the edge of the cornea to allow access to inside the front part of the eye, either surgically using a miniature diamond blade or with a femtosecond laser.
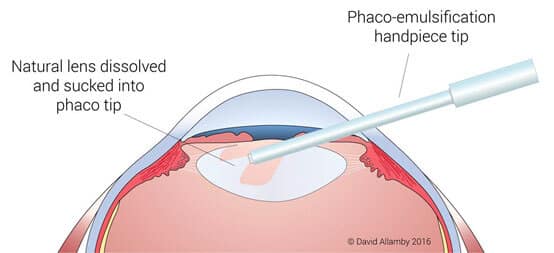
The lens is contained within a clear fibrous bag known as the capsule, which will remain even after the lens contents have been removed from within it. To access the lens material, a small round opening approximately 5-6 mm in diameter must be made in the top of the bag, called a capsulotomy. The capsulotomy can be performed using a special instrument by a skilled surgeon, or with a femtosecond laser.
An advanced ultrasound-based device called a phacoemulsification tip is inserted through the keyhole opening at the edge of the cornea, and through the capsulotomy. The ultrasound tip dissolves the lens fibres and simultaneously sucks them up the central tube within the tip.
The cataract surgeon continues aspirating the lens material from all parts of the bag. It is important to ensure no lens cortex remains as this can lead to inflammation after surgery.
CHAPTER 16
Once all the lens material has been removed, the clear opened capsular bag will remain in place, still suspended from the encircling doughnut-shaped ciliary muscle by fine fibres. The empty bag will be the new home for an artificial plastic intraocular lens (IOL).
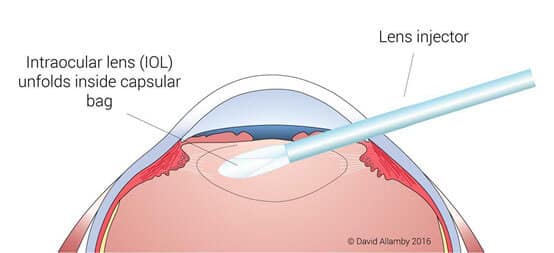
Lens Replacement Surgery Cost
Modern lenses are flexible allowing them to be folded and inserted via a lens injector, through a very small keyhole opening in the eye. Older lens implants were rigid and required a much longer incision, which would have required several stitches to close.
The benefit of keyhole cataract surgery is much more rapid healing, less induced astigmatism post-operatively (so better vision) and, because keyhole ports are self-sealing, no need for any sutures.
There are a variety of lens types that can be implanted. The choice of IOL used depends on whether surgery takes place in the National Health Service (UK NHS), where only standard monofocal lenses are available, or in a private setting where the patient can opt for advanced premium lenses.
CHAPTER 17
Once all the lens has been injected into the capsular bag, the surgeon will manipulate and rotate the IOL so that it is seated in the correct position. This will ensure the best possible vision after cataract surgery is complete. This stage is also very important for premium and toric lenses, where position and angle of the lens are vital.
Antibiotics are injected into the fluid in front of the iris, which is highly effective at protecting against bacterial infection after surgery.
Surgery is usually completed in 10-15 minutes per eye.
No sutures are needed as the keyhole entrance ports are self-sealing, removing the need to have stitches taken out at a subsequent post-operative clinic visit.
CHAPTER 18
Until recent years the only choice patients had was a standard single focus intraocular lens (IOL), known as a monofocal design. This is the lens type still used in universal health care plans, such as the NHS.

The youthful natural human lens is much more advanced, allowing us to see in at almost any distance, from far away up to only a few centimetres from the eye (when we are young).
This flexible ‘zoom’ function declines with age, a condition known as presbyopia and we need reading glasses by mid-life.
However, new optical IOL designs have created presbyopia-correcting intraocular lenses, which have revolutionised refractive cataract surgery. These implants can restore intermediate range (e.g. computer screen) as well as up close reading, such as a newspaper or phone.
CHAPTER 19
There are broadly four main categories of these advanced IOLs, which can include toric versions to correct astigmatism:

Most people who have cataract surgery would like to be less dependent on glasses after treatment. Presbyopia-correcting IOLs offer this advantage, including decreasing the need for computer glasses and reading glasses but will increase the costs of surgery.
All designs include some optical compromises and a period of adaptation will be needed. The most common complications are indistinct vision (at distance or close, or both), reduced contrast making objects appear less defined, and glare & halos around streetlights and car lights in dim-light conditions. In many cases, these issues become less problematic with time without treatment. In other cases, a follow-up procedure, e.g. LASIK or PRK may be needed to improve vision and decrease symptoms. In a small number of cases, your surgeon may to remove the presbyopia-correcting IOL and replace it with a different lens type.
Be sure to thoroughly discuss the advantages and risks associated with presbyopia-correcting IOLs with your cataract surgeon at your preoperative exam and consultation.
CHAPTER 20
There are three types of advanced lens implant designs

Multifocal;
Designed to boost computer and close reading vision ranges
Depth of Field;
Boots intermediate vision by extending the natural range that images are in focus.
Aspheric;
Allows patients to benefit from the natural residual depth of field of the cornea.
CHAPTER 21
During cataract surgery, your cloudy lens is replaced with a clear synthetic intraocular lens (IOL)
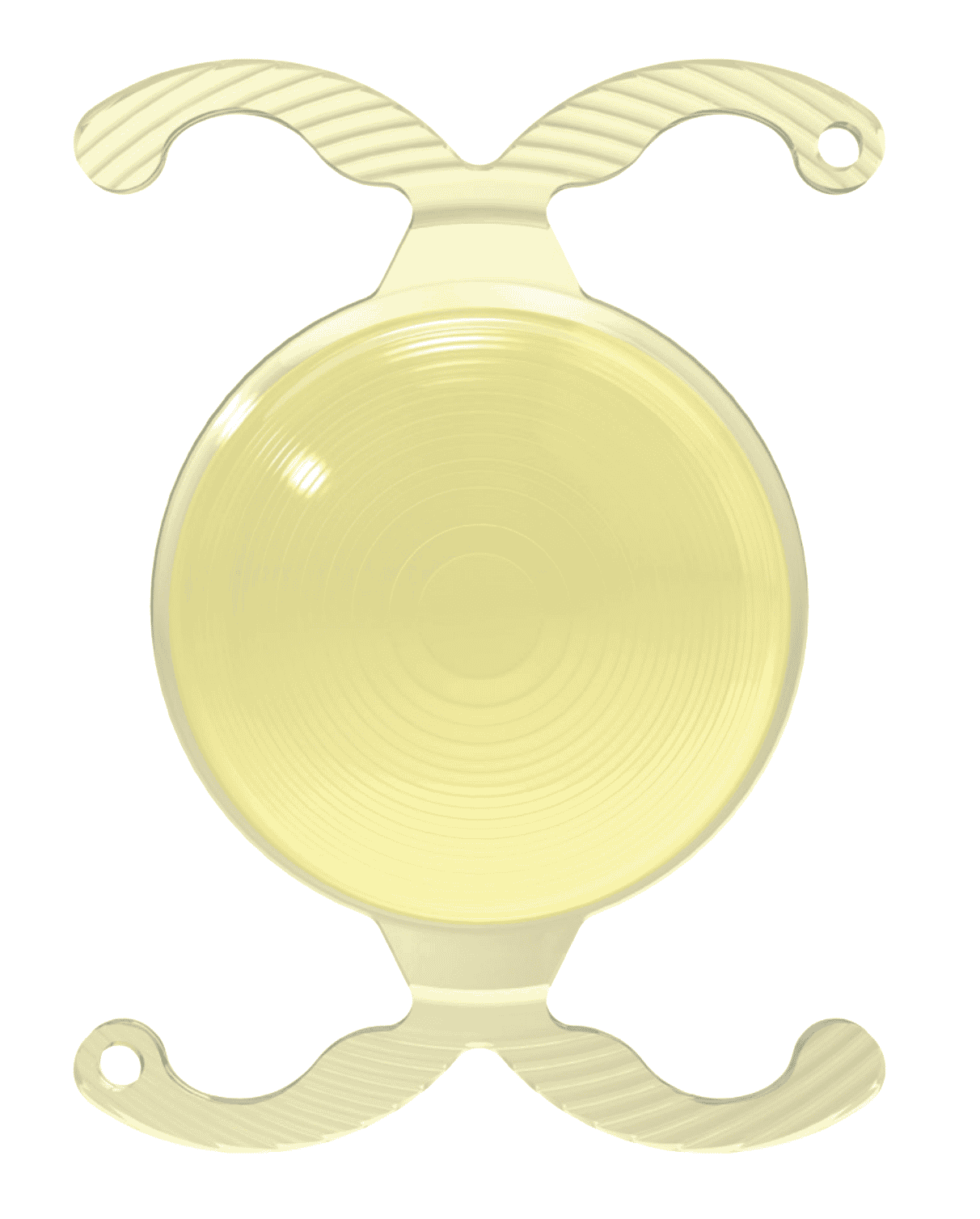
Standard monofocal IOLs only correct vision at one distance, typically to give good far vision, e.g. for driving, TV, etc. Patients would still need glasses for reading and computer use. These IOLs can also be used with monovision, with one eye for distance and the other for reading.
Premium intraocular lenses are now available that are multifocal (MIOLs) and which can improve vision at more than once distance. The image to the left shows a trifocal design to give better vision at far, intermediate and close ranges.
There are many different types of IOL. Your cataract surgeon can help you decide if you are a good candidate for multifocal IOLs at your preoperative exam and consultation.
CHAPTER 22
A newer class of intraocular lenses (IOL) has become attractive for patients who want a greater range of vision without compromising visual function.
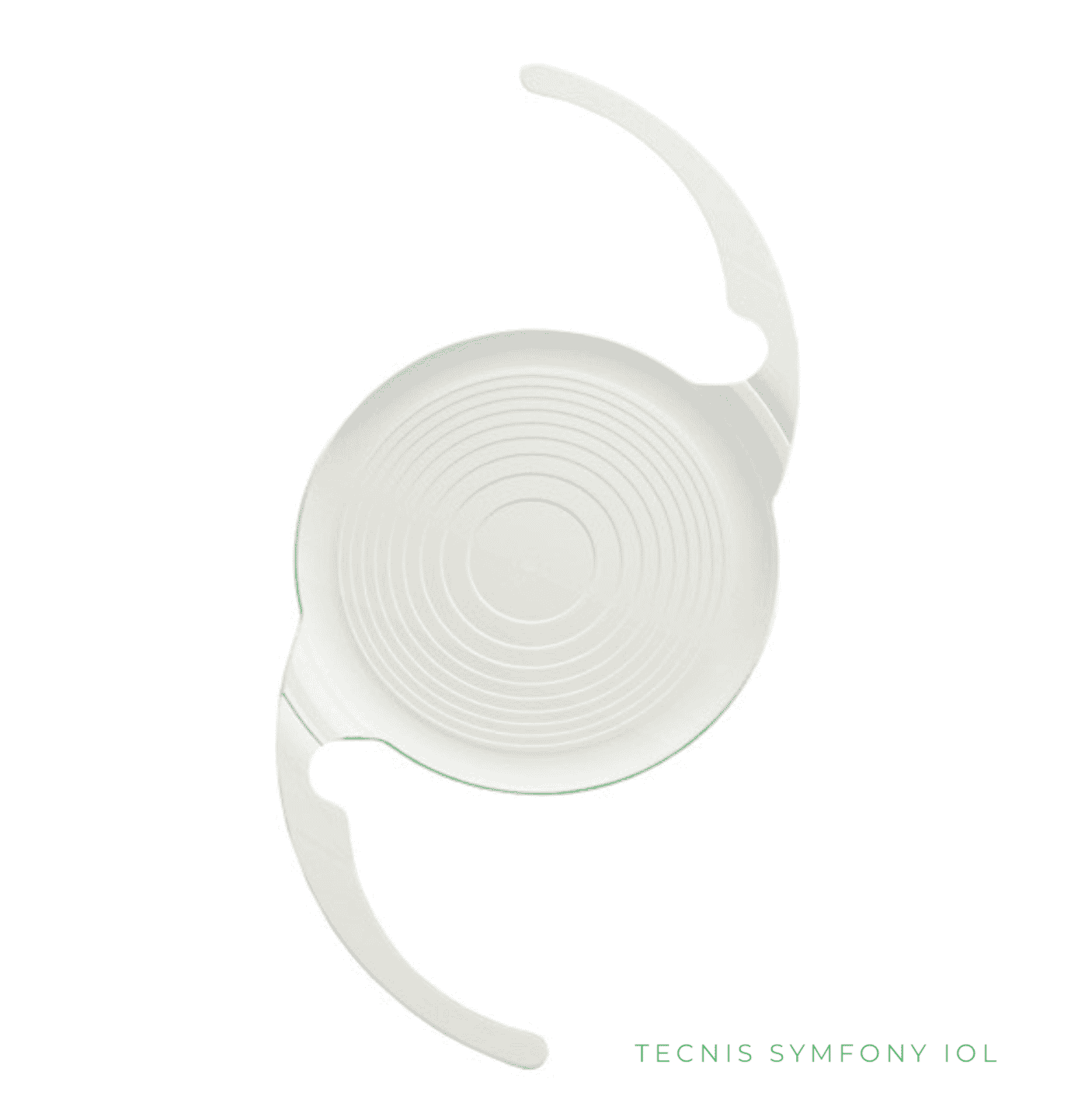
This innovative design creates a longer depth of field so that more things are in clear focus at the same time.
The extended depth of field lenses (EDFs) are useful for patients who may be unsuitable for multifocal implants, e.g. previous LASIK surgery, glaucoma and mild dry macular degeneration.
Some studies suggest that patients notice less glare and halos with EDF compared to MIOL lenses. However, EDF IOL design gives less power for close vision, and to compensate for this, EDF lens patients are often given a ‘mini-monovision’ with a slight amount of short-sight in one eye. This combination can be very effective, and your surgeon can discuss this option if appropriate.
CHAPTER 23
Accommodation is the term used for the ability of younger eyes to change optical power, altering focus from far to near and back in a fraction of a second. It is a remarkable ability which we, of course, take for granted until it’s gone (at some point in our 40s).

Accommodative IOLs (AIOLs) are designed to mimic how the natural lens allows us to see at both far and near. When trying to focus your vision through the use of the ciliary muscle inside your eye, an accommodating lens should move forward and backwards, or flex its shape to change the optical power of the eye.
The current generation of such lenses is showing some early promise, with new 2018 data showing some functional focusing that was stable out to 2 years post-implantation (with the Akkolens Lumina AIOL). Whether the mechanisms can deliver enough “accommodation” to provide clear near vision over the long-term is yet to be seen. The capsular bag can undergo fibrosis (scarring) which can affect the movement of the IOL if placed within it. In addition, the older ciliary muscle may not have enough strength or mechanical force needed to fully power the flexibility needed.
There are new lenses in development which may deliver true full ‘natural’ focusing replicating the human lens, some of which are currently in clinical trials. Most surgeons are not recommending accommodating IOLs at this time, but watch this space.
CHAPTER 24
You may be offered a choice of two surgical options: traditional cataract surgery or laser-assisted cataract surgery (LACS).
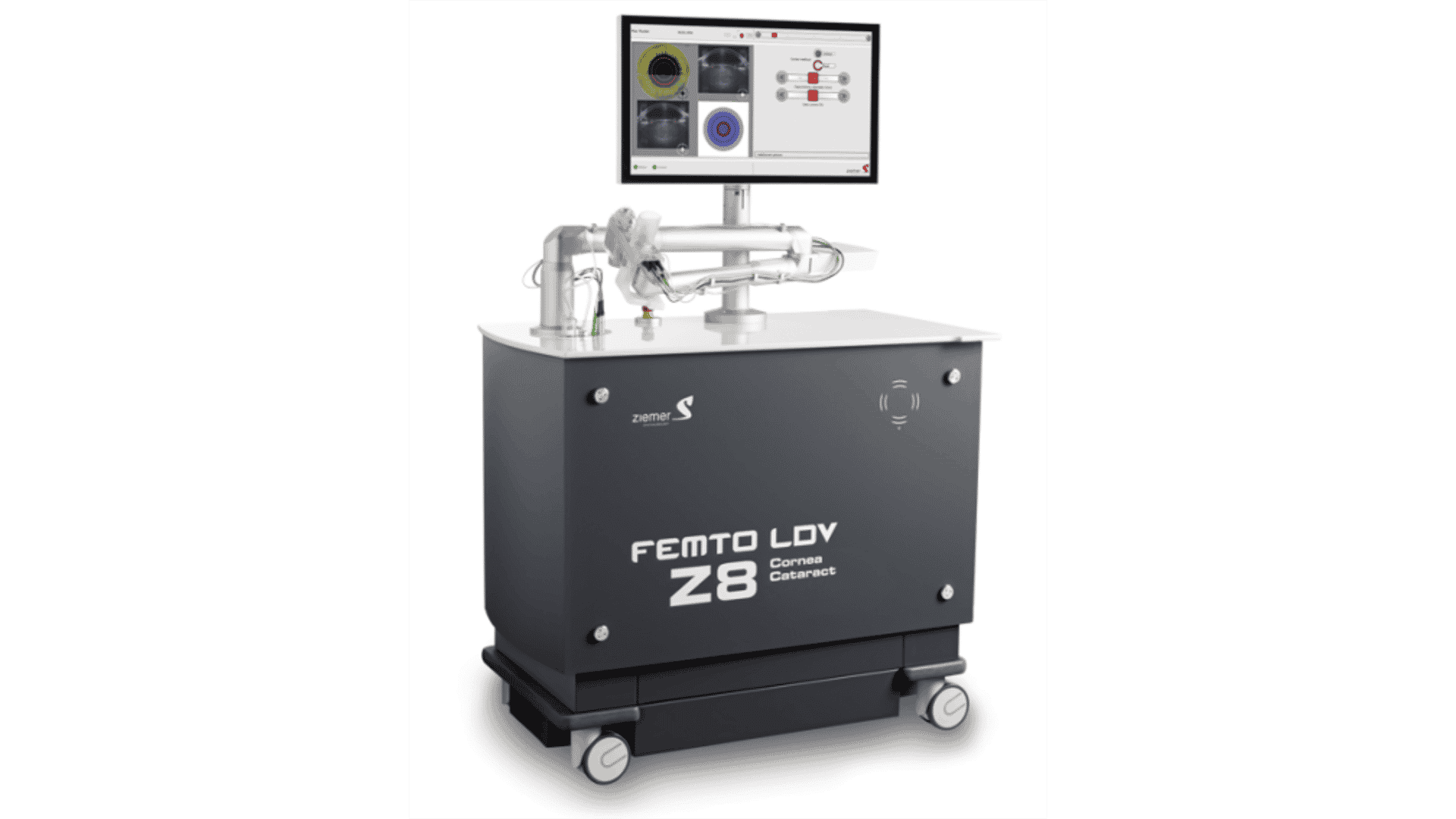
The laser is used to replace certain manual steps in the procedure including initial incisions, opening the lens capsule and dissecting the lens.
The laser option will be more expensive, but is it better? Some providers claim LACS as superior and will recommend the additional cost for its use.
However, it is important to be aware that studies have not consistently shown that laser-assisted cataract surgery results in fewer complications, faster recovery or better visual outcomes than traditional cataract surgery. With any cataract surgery, your outcome depends in large part on the skill and experience of your eye surgeon.
LACS is a technique still evolving, with its full potential yet to be achieved. It may become the standard in the future but, as of today, several studies failed to show a benefit.
CHAPTER 25
Cataract surgery is the most common and most successful surgical procedure performed today. In the US, 3 million Americans have the operation each year.

In the UK, the NHS carries out over 350,000 procedures annually.
Cataract surgery complications are fortunately not common but, like every operation, adverse events can occur and surgery should only be carried out with a full discussion of the risks and benefits.
A study of more than 200,000 American cataract patients who had surgery between 1994 and 2006 found that 99.5% had no severe postoperative complications and the risk of such events has dropped with better surgical tools and techniques.
CHAPTER 26
The most common cataract surgery complication is posterior capsule opacification (PCO).
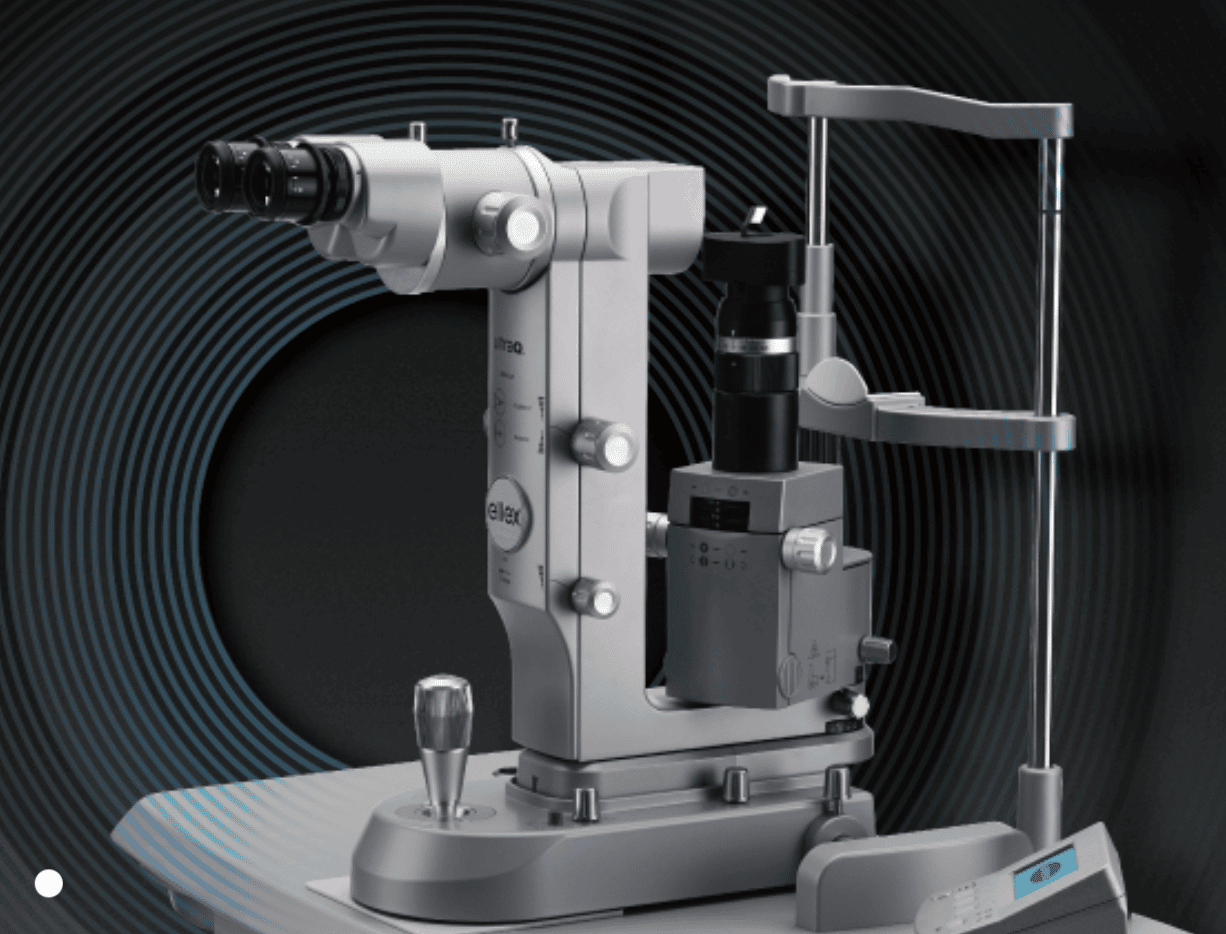
During cataract surgery, your doctor will remove the cloudy natural lens of your eye (the cataract) and replace it with an intraocular lens (IOL). The thin clear membrane bag that surrounds the human lens (known as the lens capsule) is mainly left intact during the operation. The IOL is normally implanted inside it.
However, in about 10-20% of patients, the back (posterior) part of the capsule becomes hazy some months or even years later, resulting in PCO and a reduction in vision.
Fortunately, a YAG laser can treat PCO safely and effectively. The procedure (YAG laser capsulotomy) is usually performed in the out-patient clinic. With your chin on the chin rest, a laser beam is directed at the clouded capsule behind the implant lens, and the laser vaporises the tissue, restoring clear vision. The procedure is painless and takes only a few minutes. Following YAG capsulotomy, you may resume normal activities immediately. You may experience some floaters afterwards which typically resolve within a few weeks.
CHAPTER 27
During the last 35 years, lifespan has gone up by 12 years in the West and by more than 25 years in many developing countries.
As the likelihood of developing cataract increases with age (with at least 70% of people aged 85+ affected), the medical community faces the problem of too few ophthalmic surgeons.
In 2015, around 9000 American surgeons carried out 3.6 million cataract procedures. The UK has just 1,300 consultant ophthalmologist positions, with over 90 percent of eye departments estimating that they require between one and five extra consultants over the next two years. The UK Royal College of Ophthalmologists continues to lobby for additional training jobs, but the current government position is to freeze the number of training posts for the next ten years.
Technological advancements will continue, with new IOL designs in the pipeline and refinements in how we use lasers during the procedure. Clinical trials of new gel-filled lenses are underway, though the holy grail of a true “accommodating” lens that can change its power (as can the natural lens) is still likely some way off.
The procedure is now almost unrecognisably more advanced than when, on 29 November 1949, Sir Harold Ridley successfully implanted the first intraocular lens at St. Thomas’ Hospital in London. There is no sign of the pace of new developments slowing; rather it appears to be accelerating. We look forward to what the future will hold.
CHAPTER 28
If you are looking for a specialist centre to treat your cataracts (or those of someone you know) please contact Focus Clinic on +44 (0)207 307 8250 and we will be happy to discuss your treatment options and arrange an appointment.

Call Focus Clinic on
0207 307 8250
Or email us on
info@www.focusclinics.com
Summary
I hope this complete patient guide has educated you on the causes of cataract and what might help to prevent them.
If your cataracts are still early or giving minimal symptoms, stronger glasses and better illumination when reading can help.
However, as cataracts steadily progress over time, which may be months or years, it is expected that eventually, you will need surgical treatment.
Surgery is the definitive of treatment for cataract, and to date is the only proven solution. The timing of the procedure is based upon the degree of loss of vision and how much effect that has on your daily life and activities.
The introduction of premium multifocal intraocular lenses (MIOLs) has been a major development in helping patients to get a greater range of vision after lens replacement surgery, improving both reading and distance vision.
Choosing an expert surgeon is still the most important step in your journey to living without cataracts.
Contact Focus Clinic on 0207 307 8250, and we will be happy to discuss your treatment options and arrange an appointment.