Book Your Free Consultation
Mr David Allamby
MD, FRCOphth, FRCS
LASER EYE SURGERY GUIDE
Laser eye surgery, or laser refraction surgery, refers to several procedures used to correct refraction issues within the eye.
Most often patients will be experiencing short-sightedness (myopia) long-sightedness (hyperopia) or astigmatism. With older patients showing signs of presbyopia (old-age related long-sightedness).

CHAPTER 1
As far back as the 19th century there have been surgical solutions to correct refractive errors within the eye. Radial Keratotomy (RK) was developed in 1898 as a procedure to treat short-sightedness (myopia).
During the RK procedure, miniscule incisions were made on the surface of the cornea, however, limited success was to be found with RK as it relied primarily on the skills of the performing surgeon.
During the 1990s ophthalmologist Dr. Pallikaris pioneered the use of a microkeratome alongside the excimer laser creating the laser-assisted in situ keratomileusis (LASIK) procedure. During LASIK the excimer laser is still used to reshape the cornea by removing tissue, but only once a flap has been created in the cornea with the microkeratome.
During the early 2000s developments were made to replace the microkeratome with a femtosecond laser, resulting in shorter healing times and further reducing the chance of post-surgery complications.
CHAPTER 2
What are the different options when it comes to laser eye surgery and is one better over the other?

CHAPTER 3
The public demand for laser eye surgery has risen steadily over the recent years, with an estimated 30-50 million procedures performed worldwide.
Each year approximately 900,000 Americans and 100,000 Britons have laser eye procedures.
Success rates are very high thanks to advancements in technology that have evolved significantly over the last 30 years, combined with a greater understanding of who makes a good candidate for treatment.
Improving technology and technique have made an enormous difference to complication rates, e.g. epithelial ingrowth (surface cells growing under the LASIK flap) appears to have been eliminated by the use of femtosecond laser in primary LASIK surgeries and the incidence of infection has fallen from 1 in every 3,000 cases to less than 1 in 20,000.
Increasingly, patients are considering laser eye surgery as an alternative way of correcting their ametropia (a focusing error requiring the use of glasses, including short-sight, long-sight, astigmatism and presbyopia, the need for reading glasses in middle-age), with contact lens wearers twice as likely to consider surgery than those who wear spectacles.
At Focus Clinic all potential laser eye surgery patients will undergo an in-depth screening and consultation process to determine your suitability for either LASIK or LASEK procedures.
CHAPTER 4
There are numerous reasons a patient may not be eligible for laser eye surgery, which can include issues with your overall health, or eye specific issues. Some prescription medications may also limit your suitability for laser eye surgery.

You are likely not a suitable candidate if you suffer from;
You will also be deemed unsuitable for laser eye surgery if you are currently pregnant, or breastfeeding, as there is an altered wound response during healing. Patients must wait 3 months after giving birth, or breastfeeding has ceased to be considered for laser refractive treatment.
Prescription drugs such as oral steroids, or Roaccutane/Isotretinoin can leave you at a higher risk of developing infections post-surgery. It is possible that you may be considered suitable for laser eye surgery if you are currently prescribed these or similar drugs, should the medications be stopped or substituted with GP’s consent.
Issues more specific to a patient’s eye health may also reduce their suitability as a candidate for laser eye surgery, these can include;
CHAPTER 5
Some conditions can either be pre-treated or assessed during a consultation to determine the eligibility of patients, with a decision being made whilst also considering general health and eye history.

If you suffer from any of the following you may still be suitable to receive laser eye surgery:
Excluding any pre-existing medical conditions a patient may have, there are several other factors that will determine how suitable a patient is for laser eye surgery, and the level of success they can expect to achieve with treatment.
CHAPTER 6
The ideal laser patient is over 18 years of age since any refractive errors are more likely to develop below this age. However, some patients over the age of 21 will continue to experience an increase in their prescription making them unsuitable for LASIK or PRK.

However, it seems that the average age of candidates is increasing, and during recent years the mean age of subjects receiving surgery has shown an upward trend. This is likely due to how we use our eyes in a modern environment, with ever increasing screen usage and less time outdoors.
Both factors have been shown to be linked to a progression in short-sightedness.
Younger patients, in their 20s and 30s, are generally looking to correct short-sight, with or without some degree of astigmatism. The most common choice of procedure will be LASIK, with a minority of patients having PRK.
Middle-aged patients in their 40s and 50s most often request treatment to assist with a loss of near vision. This is known as presbyopia and requires the use of reading glasses. This is often treated using laser blended vision, though patients in their 50s are also candidates for refractive lens exchange (RLE).
Patients aged 60 and over most commonly will require a refractive lens exchange (RLE), using a premium lens to correct both far and near vision. Cataracts (a whitening of the lens causing diminished vision) become increasingly common after the age of 60. The surgery to remove them is identical to RLE.
CHAPTER 7
Overall the number of men and women seeking vision correction is the same, with a consistent 50:50 split.
Both sexes show reluctance to wear glasses in certain situations. A recent poll showed that just over half of people removed their glasses when on a date or taking a selfie.

The main effect of gender is in the incidence of dry eye problems which is more likely to affect women.
A US study showed that dry eye disease (DED) affected 1 in 7 adults aged 48 or older, with approximately 50% more cases in women than men. Dry eye disease also affects postmenopausal women, those taking HRT or using the contraceptive pill.
Reliable epidemiological data from a Women’s Health Study and Physician’s Health Study indicate the prevalence of dry eye leading to symptoms in the United States is about 7% for women and 4% for men over the age of 50, which equates to around 3.2 million women and 1.05 million men with DED in the United States.
Dry eye disease is a growing problem. Twenty-five percent of patients who visit eye clinics report symptoms of dryness affecting their eyes, making it an increasing public health issue and one of the most common conditions seen by eye care clinicians.
CHAPTER 8
One of the most important eligibility criteria for refractive surgery is having stable refraction, which means that any prescription for glasses or contact lenses has stayed the same for a sufficient period of time.
This usually occurs after the age of 18 to 22 years for short-sighted patients, with or without astigmatism. Patients are often asked to produce past refraction details from their optician visits, for up to the previous 3 years, to show that they have some level of stability.

A patient with a large recent change in refraction will be advised to wait until two consecutive prescriptions are similar. The goal is to avoid patients undergoing refractive surgery and then find that a year later their prescriptions naturally became worse, leaving them once again with some degree of refraction issue.
Laser eye surgery for short-sight and astigmatism is typically very stable post-operatively and should last many years. However, if the eyes condition worsens and myopia progresses, it may incorrectly appear that the treatment has worn off.
Laser refractive surgery changes the curvature of the cornea and can correct most cases of myopia (short-sight), hyperopia (long-sight) and astigmatism. It can also correct the need for reading glasses for patients affected by presbyopia (the need for reading glasses in middle age).
Myopia is corrected by making the cornea flatter, while hyperopia is corrected by making the cornea more curved. In the case of astigmatism, the cornea is made more spherical in shape.
The amount of refractive error with good outcomes has different ranges depending on the type of prescription and the excimer laser used.

Short-sight between -0.25D to –14.00D is technically possible with the WaveLight platform, while other lasers have a lower range of correction. The limiting factor for extreme prescriptions is the thickness of the cornea, which will be measured at your consultation.
With the WaveLight system, which removes a smaller amount of tissue than some other lasers, most prescriptions up to -9.00 dioptres of myopia are treatable. Higher degrees of short-sight require a thicker than average cornea.
Astigmatism Treatment
Astigmatism can be corrected up to a severity of 6.00 dioptres. In the general population, 95% of astigmatism prescriptions are up to 2.00 dioptres, and most people have some degree of this refractive error, even if only minor, perhaps 0.25 or 0.50 dioptres.
It is less common to have no astigmatism whatsoever.
Long-Sightedness (Hyperopia) Treatment

Although newer models of excimer laser platforms allow for larger ablation diameters, the predictability and stability of hyperopic refractive surgery continue to be lower compared with myopic corrections, especially at higher degrees of hyperopia.
Other potential challenges of hyperopic refractive surgery include slower healing until the prescription is fully stable, fewer patients seeing 20/20 results compared to short-sighted corrections, and higher rates of retreatment.
The combination of these factors can reduce surgeons’ willingness to perform hyperopic refractive surgery, and most clinicians will not treat greater than +4.00 dioptres, even if the laser (as in the case of the WaveLight Allegretto) is approved up to +6.00.
If the patient is greater than 50 years of age, refractive lens exchange (RLE) may be a better option.
CHAPTER 9
Motivation for treatment should be assessed carefully preoperatively, and patients should not feel coerced into proceeding. Patients should have a cooling off period between their consultation and treatment.
Expectations should be realistic, particularly when the prescription is very high or when treating long-sightedness. Both these conditions may take longer to settle than typical short-sighted corrections.

If the only acceptable outcome from your treatment is perfect vision, then you should appreciate that no medical intervention can absolutely guarantee a perfect result. Laser vision correction produces a very high level of satisfactory outcomes but cannot guarantee perfect vision for all patients. Perfectionists may not be good candidates for any form of laser eye treatment or lens-based surgery.
Patients with obsessive-compulsive traits or disorder may not be suitable for vision correction, as expectations can sometimes be unreasonably high.
Personality also plays a role in good aftercare. You will need to be of a mindset that understands the need for regular post-operative appointments and also be compliant in taking medications and eye drops when requested.
If you feel that you are not able to either attend regularly or use drops and tablets as instructed, you should not proceed with laser eye surgery.
CHAPTER 10
Cigarette smoking has been reported as a factor in a multitude of clinical conditions that cause a dysfunctional tear film (the wet layer moistening the front of your eyes), resulting in dry eye. A recent study has shown significantly poorer tear film stability and increased evaporation of tears in smokers.

Smoking damages the ultra-thin fatty layer of the tear film. This can lead to many smokers having problems with dry eyes, including stinging or burning eyes and eye redness.
LASIK induces temporary dry eye for 3-6 months after treatment, and smoking can exacerbate symptoms.
Because of the increased risks associated with smoking and LASIK, patients are advised to refrain from smoking for at least four to six weeks before surgery and then another four to six weeks after surgery. Read more on the effects of smoking on your eye health here.
CHAPTER 11
For some, the thought of having laser eye surgery is quite daunting. Common concerns we hear from patients considering vision treatment are:

However, for eligible candidates in a specialist low-volume setting, using the latest technological advances and an expert surgeon’s skills and training. The chances of any harm coming to you through laser eye surgery is very minimal.
Some people are perfectly happy with their current vision correction solution, whether it be contact lenses or glasses. Therefore, laser eye surgery seems like an unnecessary expense.
For others, their current vision correction may not be working so well. For example, high intensity workouts or contact sports are difficult whilst wearing glasses, and contact lenses can be a hassle to put in and take out, especially when you’re in a rush.
Also, these methods of vision correction are required daily, whether it be for reading, driving, using your phone or working. More often than not, if you require vision correction, enjoying day-to-day life without them will be a lot easier!
With laser eye surgery, the procedure is:
You are given anaesthetic eye drops before the surgery, so the procedure is practically painless.
Focus Clinic has a 100% success record for 20/20 vision (or better) after having LASIK laser eye surgery for typical short-sighted prescriptions. We are so confident that our results for short-sightedness distance vision correction are permanent that we offer a Lifetime Guarantee.
If you have distance vision correction for short-sight, then any repeat laser eye treatments to correct a return of myopia in the first 10 years are included free of charge. (Terms and conditions apply, excludes any age-related changes and conditions unrelated to the primary treatment).
The cost of having LASIK surgery works out cheaper over the course of a lifetime, when compared to contact lenses or glasses. The average person typically spends £100 a year on glasses or £300 a year on contact lenses.
This means that after 10 years, you would have spent more on glasses or contacts than you would have on LASIK for typical long- and short-sight prescriptions. Considering most people with myopia (short-sight) require glasses by the time they reach their mid 20s, your lifetime spend on glasses and contacts would be £15,000 (based on 60 years glasses wear and 30 years using contact lenses). LASIK surgery costing £4,000 result in a saving of more than £10,000 in the long-term
Laser eye surgery is now safer than ever. The safety and effectiveness of treatments is in large part due to our thorough consultation and screening process.
At Focus Clinic, we only treat suitable patients, which ensures minimal complications and maximum effectiveness – we have a 100% success rate for typical short-sighted prescriptions (including most degrees of astigmatism) and a very low rate of complications.
Above all, being able to see perfectly, sometimes for the first time in your life without the aid of glasses or contact lenses is truly life changing. It lifts the restrictions that you’ve grown used to and allows you to notice all of the minute but beautiful details found in everyday life.
Don’t just take our word for it. Check out what our patients had to say about the laser eye surgery they received at Focus Clinic by clicking here.
CHAPTER 12
You may be surprised to find out that treatment will last no more than 10 minutes. Compared to our consultation and screening process it will feel as if the procedure is over in no time at all.
When you first arrive at Focus Clinic, our patient care coordinator will be on hand to greet you, and you will no doubt recognise many of the team from your consultation period. After being welcomed into the clinic, you will meet with your surgeon for review. This is a perfect opportunity to ask any questions you may have.

Your surgeon will perform some final checks, reviewing of scans and re-measuring your prescription to make sure it is correct. They will also explain what can be expected immediately following the procedure.
After all checks have been completed you will be shown to the laser suite, where one of our technicians will meet you. It is at this point that any aftercare procedures will be explained to you, what drops to use and what activities you can participate in post-surgery.
All of this information will be written down for you, our aftercare program is carefully designed so patients are regularly monitored during their first-year post-surgery.
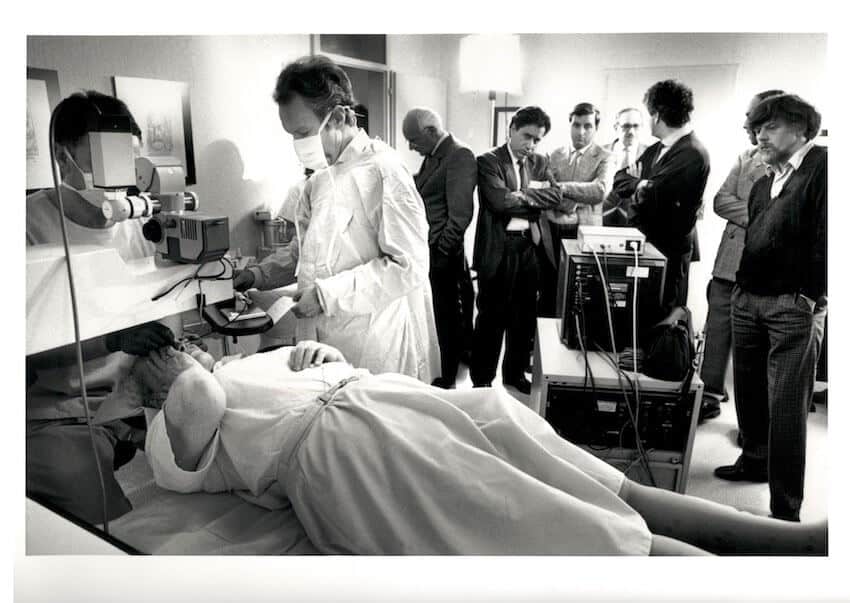
After the post-surgery procedures have been explained, you will be prepped for surgery. You will be asked to lie down on a comfortable flat bed, and your surgeon will administer local anaesthetic. This will be in drop form and takes around 5 seconds to start working.
Thanks to this, laser eye surgery is a painless experience. With most patients only reporting a slight feeling of pressure on the eye as the femtosecond laser is used to create the corneal flap.
Throughout the procedure your surgeon will be speaking to you, as you may understandably be quite nervous, they will be on hand to alleviate any fears you may experience.
Once treatment is complete, our team will take you to the recovery room. Here you will be able to lie down and relax with a hot beverage and snacks before being allowed to return home.
CHAPTER 13
Thanks to the resiliency of the human eye, and laser refractive surgery being so short and marginally invasive, aftercare following a laser eye procedure is relatively straight forward. Oftentimes patients will only experience some discomfort, generally described as a feeling of ‘grittiness’ within the eye for a few hours post-surgery.
This recovery guide should go some way in preparing you for what to expect after receiving laser eye surgery;


The morning after surgery you will have a check-up appointment, this is standard procedure to ensure everything has gone as expected and answer any queries you may have.
You will be allowed to read and watch TV again after this appointment, but you must ensure you are using the eye drops provided to keep your eyes well lubricated.
If you have received LASIK surgery you should be ok to return to work by now, if you have received LASEK/PRK you will have an aftercare appointment 3 – 4 days post-surgery as the initial healing stage will be slightly longer.
You should be clear to fly at this point, however, keep your eye drops to hand as the cabin can be an extremely dry environment.
During the night-time you may notice glare, or halos around light sources, this is completely normal and can be expected to last around a month or so.
The First Week After Treatment
Towards the end of your first week post-surgery you should be ok to begin light exercising again, such as jogging or cycling. But it will be important to prevent any sweat getting in the eyes and avoid any touching or rubbing.
If you have been cleared to drive by this point, you will need to be extra diligent if driving during the night-time. Preferably avoiding it altogether if possible.
The First Month After Surgery

If you have been experiencing halo’s and glaring at night, you should begin to notice a dramatic decrease between weeks 2 and 4. Participating in sports such as football, tennis, swimming etc is now safe.
Although impact sports such as boxing, or martial arts should still be avoided until after one month.
Eye makeup can be worn once again, but it is advisable to wait until after the first month. Focus is available to answer any questions you may have if you are unsure about which activities may be safe or not.
The First Six Months
Hopefully, any symptoms of dry eye have disappeared by now, but if not, there is no need to worry. Some patients will still need to manage dry eye with drops a few months post-surgery.
All restrictions should have been lifted by now, but we would recommend not using tanning beds until the 6 month period has passed.
Any night-time issues with haloes and glaring should have disappeared also.
CHAPTER 14

The most common complication reported post-surgery is persistent dry eyes, with published studies showing rates of up to 20-50% of patients. At Focus Clinic, correct patient selection and pre-treatment of any existing dry eye has dramatically improved these rates, dropping the post-op incidence to less than 1%.
It is important to note that women commonly suffer from dry eyes after menopause. Men can also be affected by this condition in later life.
Dry eye before laser refractive treatment can increase the risks of persistent, increased dry eyes.
If your eyes are very dry beforehand, your risks are increased and it is likely better to avoid laser vision surgery. Another option for selected short-sighted patients is an ICL (implantable collamer lens) with far less risk of induced dryness.
There is an exceptionally rare chance of infection (seen in only 1 in 10,000 cases). However, this rate is still lower than that of contact lens users (1 in 2,000 cases). Making contact lenses 5 times more likely to cause loss of vision from micro-organisms compared to LASIK.
Impaired night vision such as halos or glare can often occur after laser treatment and is linked with the degree of prescription treated; it is most often seen in the high and extreme myopia cases, typically of -8.00 dioptres and higher.
Having a normal or small pupil in the dark appears to reduce the chance of developing night vision difficulties. A better option for some patients with very high prescriptions is an artificial lens replacement, known as an ICL (implantable collamer lens).
ICLs have been a major breakthrough for extreme myopia, with much less chance of night vision problems.
Problems Associated With The Corneal Flap

Laser eye surgery involves making a precise layer of separation in the cornea using an instrument called a femtosecond laser to create a flap. Another laser will then be used to reshape the corneal tissue underneath. Once the tissue has been corrected, the flap will be put back into place.
If the flap wasn’t made properly or you don’t follow best practices recommended by your clinician following the surgery (such as avoiding getting water in or frequently rubbing your eyes), flap issues can occur. This can affect the way the corneal flap heals and lead to:
While this complication is common with blade-cut techniques, the advent of modern femtosecond laser LASIK has reduced the incidence of epithelial ingrowth to zero percent with the primary procedure. If a re-treatment is needed (in one to four percent of cases), mild ingrowth can be seen, and treated.
Or, a treatment called corneal collagen crosslinking may be required to strengthen the cornea.
Reducing The Risks Of Laser Eye Surgery

The main safety factor surrounding laser refractive surgery is selecting patients who are good candidates for treatment. In 2015, most complications arose when the person treated was not an ideal candidate.
This will come down to the surgeon and clinical setting. If it is a high-volume commercial environment where less time is spent on assessment and selection, the level of risk will increase.
Choose a specialist surgeon in a low volume setting, such as a clinical-owned specialist centre. There are always possible risks with any surgery, and we encourage you to discuss these with us.
Serious complications with PRK or LASIK are very rare if patients have been well selected. The chance of experiencing complications from LASIK has been documented in clinical studies to be less than one percent. Based on procedures performed using less sophisticated technology than we have today.
Many of the risks and complications associated with this procedure can be reduced or eliminated through careful patient selection and thorough pre-operative testing using the latest diagnostic technology. This is why Focus has invested so heavily in screening technology.
After laser eye treatment, you may experience some visual side effects. These are usually mild and most often diminish over a few days to a few weeks. But there is a slight chance that some of these side effects won’t go away completely, such as feelings of dryness, glare and halos.
If, after a thorough examination we decide you are a good candidate for vision correction, you will be given additional information about the procedure, allowing you to make an informed decision about whether to proceed.
These complications sound scary, we know. But it’s important to realise that they’re very rare, occurring in less than half a percent of laser eye surgery cases. With many complications suitable for correction.
The advent of new technologies has revolutionised the landscape of complications with the laser eye surgery. For example, ectasia is now treatable with collagen cross linking and epithelial ingrowth has been eliminated as a complication of primary LASIK procedures.
In addition, LASIK eye surgery is not only the most common form of laser eye surgery. It’s also the safest and most effective.
The benefits of laser eye surgery outweigh the (very rare) chances of complications by a large margin.
CONTACT US
If you’re interested in learning more about laser eye surgery, don’t hesitate to drop us a message. Focus Clinic is the only laser eye surgery clinic in the UK with a published 100 percent success rate.
We’re also the most trusted clinic in the country, as indicated by our reviews.
Our two surgeons have over 45 years of experience and have performed over 35,000 procedures between them.
We also offer a comprehensive aftercare package with a unique 10-year guarantee.